Retina Examination
Examination of the retina can offer a spectrum of difficulties. It can be straightforward and easy in the young, cooperative patient without coexisting ocular disease, and it can be extremely challenging in some patients who are less cooperative and/or have coexisting eye diseases that preclude optimal examination.
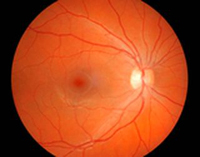
A retina exam is focused on the back of the eye. For this reason, the doctor will spend a lot of time looking through your pupil at the vitreous, retina and other structures located inside the back portion of the eye. Every patient can expect to have their eyes dilated so the doctor can get a clear view of these structures.
The following methods are normally used in diagnosing retina problems:
Indirect ophthalmoscopy uses a specialized microscope that allows the doctor to observe the vitreous, retina and other internal structures in the eye. The ophthalmoscope is probably the first instrument you will see used by the doctor during your exam because it provides an overview of the situation.
A visual field or perimetry test measures the ability of your eye to see straight ahead and to the side (peripheral vision). During a visual field test, one eye is temporarily covered and the patient is asked to look straight ahead at a fixed space. There are two kinds of tests: a moving target test and a fixed target test.
In the moving target test, the targets are moved from the side, where they are not visible, toward the center of vision until the patient sees them. This test can be performed with either a black screen on the wall or with a large bowl-shaped instrument.
A fixed target test, called computerized static perimetry, uses small points of light that appear bright or dim but do not move. During this test, a patient sits in a chair facing either a bowl-shaped instrument or a computer screen.
The visual field examination detects “blind spots” that may be caused by diseases of the retina.
